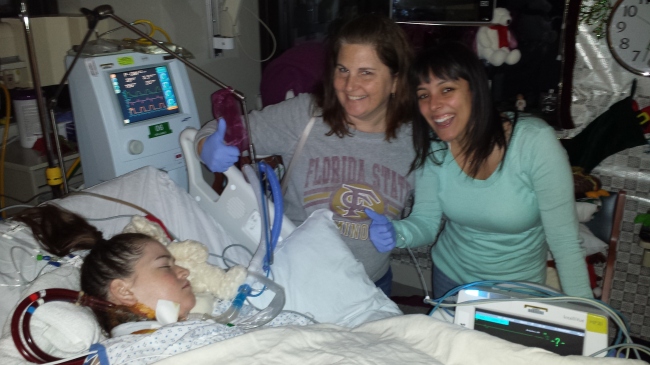
So it’s now 2:39 pm and the surgeon came in about 30 minutes ago and let us know that Jordan is headed to recovery! He even informed us that she is no longer on the ECMO machine, which was great news to us because it had been indicated to us that she would probably need to stay on that machine for a couple days following the transplant. The fact that she is off of the ECMO is fantastic because it means her new lungs are functioning well enough on their own already, That’s a wonderful sign! The next couple of days are going to be a critical time for Jordan. Typically, this is the time it takes to see whether the lungs are going to be accepted or rejected by the body. So, give us 48 hours so we can report to you again how amazing and strong the “Warrior (Jordan)” is!
Monthly Archives: December 2013
Out with the old, in with with new!
“Not really scared, just nervous and tired” – Jordan this morning as they were prepping her for surgery.
We got the call we’d been waiting almost three weeks for yesterday as we sat for dinner at our dinner table (a kid table with little baby chairs in the corner of the CVICU waiting room). The Transplant Doctor called Darrell around 6 pm; “The moms” didn’t think it was a big deal because he had been calling Darrell twice every day to give updates on Jordan’s status, so they just kept eating. Shortly after taking the call, Darrell comes in, all too calmly, and says, “We got an offer on some lungs. Jordan is scheduled for surgery tomorrow morning at 6.” “WAIT WHAT?!?!?” Darrell had to repeat what he said because we were in such shock. We had just gotten used to just maintaining life without any progress for the future. We all ran in to tell Jordan and she was excited. Darrell informed Jordan that it is typical to have one or two “dry runs,” which means they get an offer on lungs but for one reason or another the lungs are not deemed good enough by the transplant team. So Jordan, being the mature 18 year old that she is, told her mom to “calm down.” And so we did.
It’s such a difficult situation, the emotions you feel when you learn the lung transplant is taking place the next morning are so conflicting. On one hand you are super excited because this new lungs are the only chance that Jordan has at a continued life. On another hand, the surgery itself is very risky, so of course we were scared. And also, you can’t help but think about the family who had to make the extremely difficult decision, accept a loss, and to donate the organs of their loved one. Our hearts go out to that family. I don’t know how we all haven’t had any heart attacks with this roller coaster ride we have been on the past couple weeks. But, there we were. So we kissed her good night and went home (except for Darrell who stayed with her) to get a little shut eye, as much as we could given the circumstances.
So this morning we were all there by 5:30 am just talking to Jordan before they came to take her. The doctor called Darrell around that time to let us know that the lungs were local and he was going to go and personally look at them to make sure they were good enough. We really don’t know if we could have handled a false alarm.
Around 7 o’clock, the nurses along with probably 10 other people were in the room preparing Jordan for surgery. The doctor came over to us and said that the lungs looked great and they were going through with the surgery. We were so excited we couldn’t contain ourselves. As they were wheeling her away toward the operating room all of the other CVICU staff that had taken care of Jordan and had grown to care about her were telling us good luck and smiling just as big as we were! We watched them wheel her in and said, “We love you Jordan! You are a Warrior.”
Now here we are….sitting in the waiting room with family and friends. The doctors told us to go take a long breakfast and distract ourselves. Good luck with that….we got Dunkin Donuts brought over by some close friends and we are camped out in our usual spots. In approximately 6 hours, we shall know more. So until then….”just stay calm”
WAITING FOR A MIRACLE BEFORE CHRISTMAS
So this is Jordan’s family again. We are becoming increasingly desperate. Jordan has fought so hard, and overcome so many obstacles, but her time is dwindling the longer she remains on life support. Her strength and passion for life has been such an inspiration to not only her family but to everyone her story, her life, has touched. We have prayed continuously for a miracle, but time is truly becoming our enemy. Please keep Jordan in your prayers. Jordan has an amazing transplant team here at Florida Hospital and we know that, with a set of lungs, Jordan will have a shot at a full and complete life.
We wish we could get people to understand the importance of organ donation, not just for Jordan but for all people who are awaiting transplantation. It’s a tough conversation because, on one hand, we are attempting to gain by someone else’s loss. The only difference is that Jordan’s life can be saved, while the donor’s cannot. We by no means wish any harm to anyone but we know that death and disease occurs every day and no one has control over it. What you do have control over is hearing our plea and taking time to consider all of the lives that can be saved by the miracle of organ donation.
UPDATE on our warrior, Jordan
So it’s been 7 days since Jordan’s last post. Which, if I may, I would like to describe the situation Jordan was in at the time of the that post. Jordan had been in the hospital for three days, and she hadn’t had the desire to post anything. We had no prospects for lungs because she wasn’t yet on any transplant list. So at that point the doctors said to us, in exact words, “The CO2 will put her into a CO2 narcosis. This is a good thing for these patients; they will just fall asleep and not wake up.” You would think I’m lying, but I’m totally not. We were not prepared to hear that. I mean, Jordan was just at home 3 days earlier watching football. When people said that the end stage would happen quickly I think we all subconsciously slowed down our idea of what “fast” really meant. Looking back, we all know that the “start” of this end stage was really in October, when Jordan and Logan were in the hospital for two weeks over Halloween and their sister, Meghan’s birthday. They were both sick but Jordan had had her first collapsed lung. At the time we didn’t realize that the collapsed lung meant the beginning of this phase….now of course we do. Okay, so back to my story about Jordan, she hadn’t posted anything since November 27 and it was now December 11. Again, we had just been told to let her “go to sleep.” We had a family meeting with Jordan’s CF doctor’s about trying to get her transferred to a transplant facility to get her fast tracked to the list. Shand’s, who we originally had spoken with about Jordan and Logan, wouldn’t take her as a transfer until she was discharged…which was likely not going to happen. So that was where we were….practically hopeless. UNTIL, the primary CF doctor asked if we would be interested in Florida Hospital South, which was not, at the time, covered by our insurance. We didn’t care, we were willing to pay whatever it took to give our daughter a chance at life. The doctor made some calls and a few hours later he came in to Jordan’s room, leaned in real close to her ear and asked her, “Are you ready to fight?” Jordan nodded her head while he told her that Florida Hospital South had agreed to take her on as a consult and try to get her on the list for a lung transplant. Once the doctor walked out, Jordan sat up and said, “Where’s my computer? Where are my glasses?” We all started cheering that she was finally able to find something worth writing about. She was transported at midnight that night.
Florida Hospital South was a little bit of a culture shock. Nemour’s is so family oriented and treat everything with “kid gloves.” Well once we spent just 12 hours at FH South, we no longer wanted those kid gloves. The transplant team was in Jordan’s room by 7 am the next morning talking about what needed to be done to get her listed ASAP. All day consisted of tests and pokes and prods, one after another, in an effort to get her evaluation done to see if the she was eligible for transplant.
Jordan was still on the BiPAP machine at this point, we were always told intubation, chest tubes, and tracheotomies were a no-no with CF patients so as far as we were concerned, she was going to stay on BiPAP for as long as it took to get new lungs. That idea was short lived. Thursday night Jordan’s dad had spent the night, like he does every night, and early Friday morning calls started coming in from him that the doctors were getting ready to intubate her. Everyone rushed over to the hospital knowing that intubation for CF patient was not good and that if the doctors had agreed to do it, the situation must be bad. Her CO2 was continuing to rise on the BiPAP so they had no other choice, Jordan’s lungs just couldn’t do the work. She was sedated most of Friday and into Saturday…until of course the next big loop of that roller coaster we were riding came. The intubation/trach wasn’t enough, again her CO2 was rising, they had to do an ECMO (artificial lung). ECMO stands for Extracorporeal Membrane Oxygenation. ECMO is used when medicine and the breathing machines have failed to provide the support needed for the lungs, and that’s where our Jordan was at.
With all of the treatments and machines that Jordan had been on, we were told she had rated higher on the transplant list than anyone that the transplant team had seen. That sounds good right?! Well…it’s been four days since the ECMO was placed and there have been no calls about any lungs being available. So that’s where we are, waiting for the call that someone else’s untimely death will provide Jordan with new life. We are hoping for a Christmas miracle.
Also, thank you to everyone for your well wishes and prayers on Jordan’s behalf. She is, and will continue to be, in need of all those wishes and prayers in the coming days and weeks.
– Jordan’s family
Dramatic turn in events
I apologize in advance for the lack of posting and the obvious errors that will be in this post. Its only 8:30 but I feel like I’ve been up for days. It all started about a week and a half ago. I got a really bad cold. Yeah, any normal person can say that colds suck. But for CFers, a cold can lead to pretty bad chest infection that is hard to recover from. Thats what happened to me. My chest started to produce more mucus so my mom called to the doctor to get an antibiotic so it wouldn’t get worse. But the damage was done. My lungs were not expanding as much and I could barely walk from point A to point B. On Sunday, I suspected it might be a pneumothorax. My Dad, Sheena and I went to the Nemours Emeregency Room. Logan and I had our first evaluation at Shands scheduled for Monday, December 9th, so by going to the ER there was no way I was making that appointment and who knows when the next one would come.
So they confirmed I had a moderate pneuomothorax on my right side.Then I started coughing up blood a little later into the night. That’s never fun. At first they thought it was just a side effect of one of the painkillers, but an x-ray showed a lot of white fuzzies which suggetsted internal bleeding. So not only do I have a collapsed lung, I am bleeding into my other one. The least invasive procedure for the pneumo is oxygen and time. However the doctors were really concerned with the bleeding. My heart was beating about 145 bpm and my respiratory rate was 45. My oxygen was still mid to low 90s. The solution: A BIPAP. Its basically this machine that helps breathe for you. So good for my body. Not so good for my disease progression. Talks in hushed voices ensued between my parents and doctors.
Basically: My disease has declined rapidly in the past few weeks. I need the BiPAP machine so that my body doesn’t wear out. If the BiPAP doesn’t work for some reason, I may have to be intubated. This means that a tube is put down my throat, I am put asleep, and a machine breathes for me. The chances of a CFer waking up are slim to none.
My family was facing hopelessness. The doctors and social worker came in and spoke to me about my options. I wanted to try all available options before being intubated. That seems so final. But I was afraid. Hell, I still am. What about transplant? Would this make me ineligible? I am not afraid of death; I just don’t think its my time yet.
My doctor was able to get in touch with Florida Hospital. They agreed to transport me tonight and determine eligibilty. So hopefully within the coming days we will know. This whole process moved up much faster and a lot scarier.
I would like you all to pray for me and my family. I would really appreciate it.
Sorry if this was confusing. Comment with any questions.